Inner-Ear Barotrauma vs. DCS
One of the conditions that is more likely to occur in technical and mixed-gas diving is inner- ear decompression sickness (IEDCS).
Technical diving, and technical mixed-gas diving in particular, presents divers with increased risks and a unique set of hazards. Mixed-gas divers need to manage complex equipment, multiple breathing gases, and mitigate their risk of narcosis and the hazards caused by increased gas density by replacing some, or all, of the nitrogen in their breathing gas with helium. This use of high-content helium gases requires special considerations for gas switching and an adjustment of ascent rates and decompression time, and it can pose additional risks.
IEDCS has been shown to be most common in deep trimix and heliox diving, and while presentation appears similar to inner-ear barotrauma (IEBT), treatment of IEDCS requires dramatically different pro- tocols. Both IEDCS and IEBT can cause permanent damage of the inner-ear if not treated promptly, but IEDCS can be associated with neurological manifestations of DCS and can be life-threatening. Protect yourself and respond to dive injuries more effectively by knowing the difference between the two conditions, and how you can respond to them.
Inner-ear barotrauma
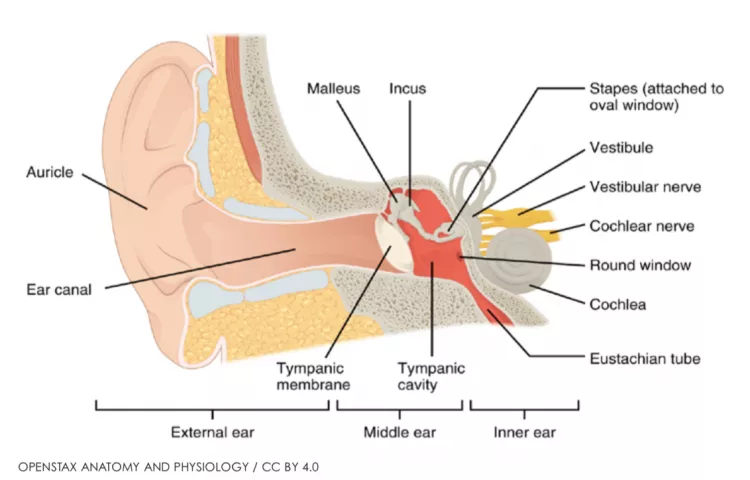
Inner-ear barotrauma is a pressure injury of the inner ear that is caused by pressure differences created through incomplete or forceful equalization. The injury can include round-window bulging or rupturing, and leakage of inner-ear fluid, which can lead to damage of the hearing and balance organs.
IEBT will heal spontaneously in many cases, but if a fistula is created it may require surgical repair. Damage can be caused to the inner ear without a rupture of the round window, but if a rupture does occur, loss of fluid from the inner ear can lead to permanent hearing loss. Symptoms of IEBT include severe vertigo, hearing loss, tinnitus, involuntary eye movement, and a feeling of fullness in the effected ear.
IEBT has two common mechanisms of injury, one from inadequate equalization, and one from equalization that is performed too forcefully. The inner ear is separated from the external world by the middle ear, and if the middle-ear space is properly equalized, the risk of inner-ear barotrauma is extremely low. If the middle-ear is not equalized during descent, however, the water pressure on the eardrum can transfer through the ossicles of the middle ear to the oval and round window of the ear. This pressure can cause the round window to bulge outward, and if the pressure is great enough, the window or the tissue surrounding it can tear.
In its other mechanism of injury, IEBT can be caused by excessive equalization, specifically via the Valsalva maneuver, which can increase intra-cranial pressure and cause pressure waves in the inner ear and outward bulging of the round window. The pressure waves alone can cause damage to the inner ear, and a rupture of the round-window can exacerbate any injury.
Inner-ear decompression sickness
IEDCS can occur after long or deep dives, after rapid ascents, or after a change in inspired inert gas is made, from helium to nitrogen. It was previously thought that only deep divers using mixed gases could suffer from IEDCS, but recent incidents have shown that the condition can afflict recreational divers performing dives as shallow as 90 feet.
Divers performing deep dives and switching from gases whose inert content is primarily slowly diffusing nitrogen, to quickly diffusing helium, put themselves at increased risk. Helium diffuses into tissues faster than nitrogen leaves and this may create a supersaturation condition that results in increased bubbles.
Between 70% and 80% of IEDCS cases involve a patent foramen ovale (PFO), and there appears to be a strong relationship between the two conditions. Evidence has shown that IEDCS is most likely to occur in individuals who have a significant venous bubble population, a large PFO, a mechanism to cause a right-to-left shunting of the blood through the heart, and measurable tissue supersaturation.
Venous bubble population and tissue supersaturation can often be found in technical divers after long or deep dives. The poorly perfused inner ear, particularly the vestibule, once saturated, can take a significant amount of time to off-gas and remain supersaturated for a period of time, which can increase the risk of IEDCS if it coincides with venous gas bub- bles passing through the PFO.
Emergency response
It can be very difficult to determine whether an individual has been afflict- ed with IEBT, IEDCS, or both. Both may present with vertigo, nausea or vomit- ing and hearing loss, and discernible signs of middle ear barotrauma may be absent. IEDCS will, more often, afflict the vestibular portion of the ear, resulting in severe vertigo, while IEBT will most often affect the cochlea and cause deafness, although in many cases both symptoms present simultaneously.
Injured divers who present with any symptoms of IEDCS after a dive should be assumed to have DCS, and should be administered emergency oxygen and brought to qualified medical care as rapidly as possible. Physicians treating the injured diver may be able to accurately diagnose one condition, but in many cases will assume the presence of DCS and treat accordingly, with recompression and associated interventions. Divers who are afflicted with both IEDCS and IEBT can have good outcomes, as long as the response and following interventions are adequate and timely. In most cases, there is some residual damage, which improves over time.
For more information on ear injuries and safe diving practices, visit DAN.org/ Health.
- Log in to post comments